As a contribution to help COVID‐19 Patients, Researchers at TU Wien designed a simple oxygen device.
It consists of only a few simple parts and could be ready for use in a short time: A new type of
oxygen device is designed to help COVID‐19 patients breathe.
One of the biggest concerns currently related to the COVID 19 epidemic: intensive care units have a
limited number of ventilators. At TU Wien, an oxygen device was therefore developed that is based
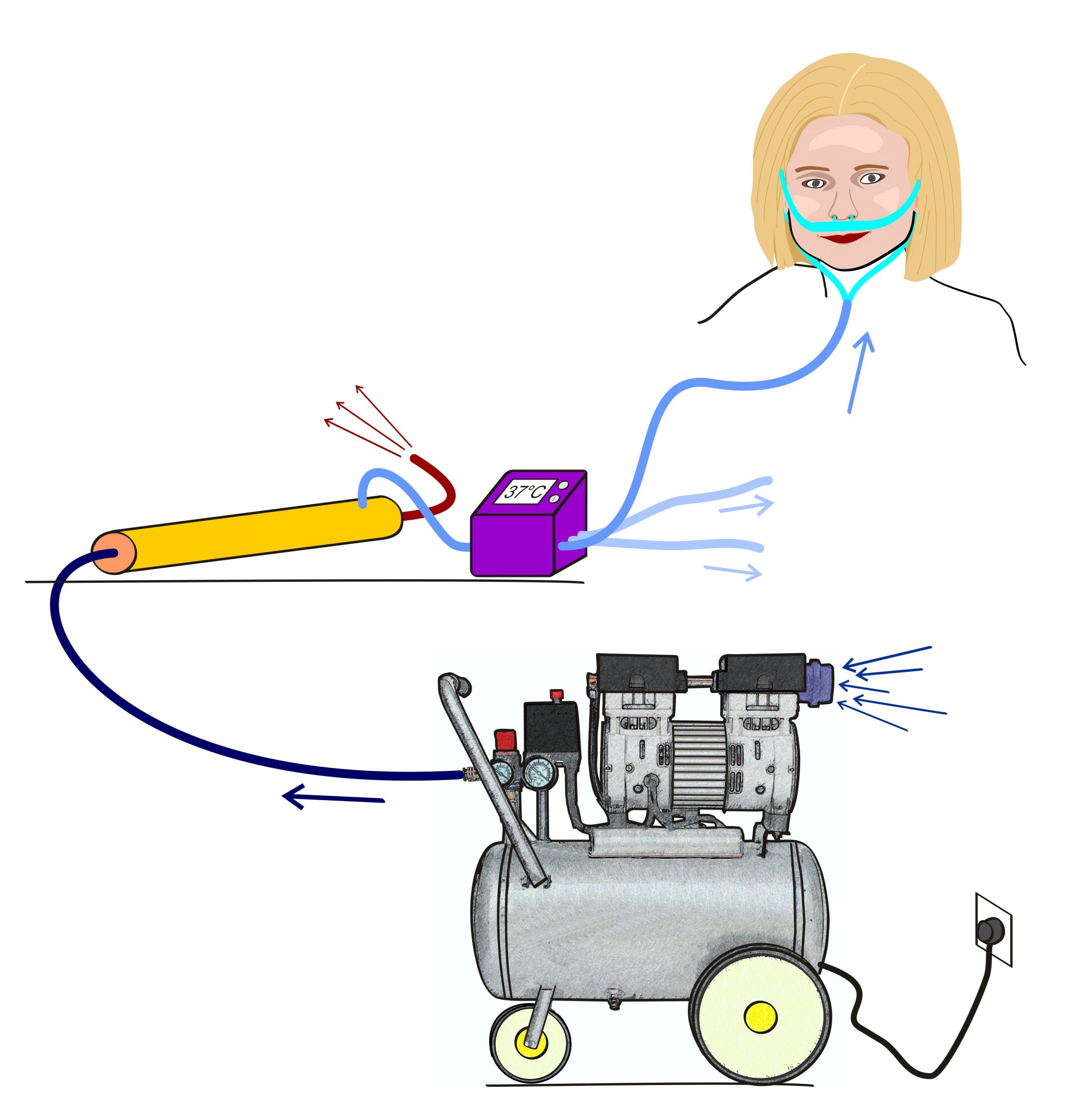
on simple, approved and tested components and could be assembled in a few days. The air that
comes from a commercially available compressor is enriched with oxygen using a special membrane.
This oxygen‐rich air can then help patients with severely affected lungs to breathe.
Such therapy, which can be started at an early stage of inpatient care, could delay or completely
avoid intubation and ventilation with a conventional ventilator. This method could help to save
valuable resources, especially if many patients with breathing difficulties have to be cared for at the
same time. Depending on the compressor and membrane separation capacity used, a single device
could supply 20 people or more at the same time.
More oxygen, higher pressure
The design for the novel oxygen device comes from Prof. Margit Gföhler, head of the Research Unit
for Biomechanics and Rehabilitation Engineering (Institute of Engineering Design and Product
Development, TU Wien) and Prof. Michael Harasek, who has been at the Institute of Chemical,
Environmental and Bioscience Engineering for many years, deals with membrane technology. They
received medical advice from the specialist for respiratory medicine Dr. Alexander Aloy (intensive
care physician and lecturer at TU Wien).
When the lungs can no longer supply the body with enough oxygen, support is needed. There are
different possibilities. In extreme cases, there is need for intubation and use of a ventilator. In many
cases, however, it is sufficient to support the lung function by providing the patient with a sufficiently
strong air flow with a high oxygen content. This is exactly what can be achieved with a relatively
simple concept.
„Most of the components of our device can be found in a normal hardware store,“ says Margit
Gföhler. You need an oil‐free compressor, an air filter, the piping and a container to humidify the air ‐
and a module with a special membrane to increase the oxygen content. „This membrane is the only
component that is not so common ‐ but these membranes are also not unusual in industry today,
they are commercially available in sufficient quantities,“ Michael Harasek is convinced.
Membrane technology: separating oxygen from nitrogen
Harasek has been working on membrane technologies for separating gases for a long time:
“Normally, air is passed through such a membrane in order to obtain nitrogen and separate the
oxygen. This is a technique that has been known for a long time. We just have to reverse this
principle here: We do not use nitrogen, but rather the enriched oxygen.” In this way, an oxygen
concentration of approx. 40 % is achieved. The oxygen flow can be set variably for the patient at up
to 60 L / min. However, excessive oxygen flow due to possible aerosol formation should be avoided.
Target SpO2 should be (according to a recommendation of the Robert Koch Institute from March
2010) > 90 % in adults and 92‐95 % in pregnant women (WHO guidelines). The air is then
thermostated and humidified and passed into the patient’s nose with increased pressure via two
silicone tubes or a breathing mask. A single compressor can supply oxygen‐enriched breathing air for
several COVID‐19 persons that require oxygen enriched air treatment.
A key advantage of the device is that it does not need oxygen bottles ‐ the oxygen simply comes from
the ambient air. “This is important because it is very difficult for hospital staff to always keep an eye
on which oxygen bottles need to be replaced. And supplying a sufficient number of oxygen bottles
can also be difficult,”says Michael Harasek.
„We are already talking to companies that are interested in this technology,“ says Margit Gföhler.
„From our point of view, it is technically possible to put such devices into operation in a short time if
it should be necessary and the technologies currently available in hospitals are no longer sufficient.“
The device is new, but the effect it does is a medically recognized measure: „We know that adding
oxygen‐enriched air can be very helpful for COVID‐19 patients with breathing problems,“ says
Univ.Doz . Dr. Alexander Aloy.
Literature:
1. Physiotherapy Management for COVID‐19 in the Acute Hospital Setting: Recommendations to guide clinical practice Version1.0 23 March 2020
2. Hinweise zu Erkennung, Diagnostik und Therapie von Patienten mit COVID‐19“ Stand März 2020 Robert Koch‐Institut: unter „Allgemeine Maßnahmen bei stationärer Versorgung“ als Empfehlung: „Sauerstoff‐Gabe (nasal, Maske, ggf. High‐flow)“.
3. Consensus statement: Save Airway Society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. The Medical Journal of Australia ‐ Preprint only;17 March 2020; David J Brewster et al.
Contacts:
Prof. Michael Harasek
Institute of Chemical, Environmental and Bioscience Engineering
TU Wien
Getreidemarkt 9, A‐1060 Wien
T +43‐1‐58801‐166202
michael.harasek@tuwien.ac.at, biofluidslab@tuwien.ac.at
Prof. Margit Gföhler
Institute of Engineering Design and Product Development
TU Wien
Getreidemarkt 9, A‐1060 Wien
T +43‐1‐58801‐30615
margit.gfoehler@tuwien.ac.at, biofluidslab@tuwien.ac.at
Univ.Lektor Dr. med Alexander Aloy
Institute of Fluid Mechanics and Heat Transfer
alexander.aloy@tuwien.ac.at
Aussender:
Dr. Florian Aigner
PR and Marketing
TU Wien
Resselgasse 3, A‐1040 Wien
T 0650 5256414
florian.aigner@tuwien.ac.at
https://biofluidslab.tuwien.ac.at

